The tips below explore how you can convince leaders that a strong compliance culture adds value to the organization. These best practices can help you establish a healthy compliance culture with effective training and measurement and, in turn, enable your organization to better manage and control risk.
Continue readingFour Power Skills for Influence
Compliance helps healthcare organizations mitigate risk by building strong relationships and leading through influence for effective regulatory change management
Continue readingDecide: YouCompli helps your organization make easy regulatory decisions
Before YouCompli, Compliance Officer Scott Borsuk said he “probably spent six to eight hours a week reading regulations, then copying and pasting them” to share with colleagues. Read the Western Maryland Health System case study.
“It’s not enjoyable reading,” Borsuk noted.
But he had to read closely to be sure he properly analyzed the regulation to see if it applied to him.
Simplify decision-making
“We were not confident that we were catching everything, we had the documents but didn’t know if we missed anything. At the end of the day, we didn’t know if we were making the right changes or not.” – Scott Borsuk, Chief Compliance Officer
Borsuk knew he needed a better system and a stronger approach to managing regulatory change. That’s where YouCompli came in. With YouCompli, Borsuk can easily decide if a regulation applies to his hospital system and how to comply.
YouCompli makes it easy for you to decide which regulatory changes apply to your organization and which tasks need to be performed in order to comply.
In this clip Scott Borsuk explains what regulatory change management is, and how YouCompli assisted his hospital system in achieving desired results.
Watch more videos on this topic here and see how YouCompli can help your organization
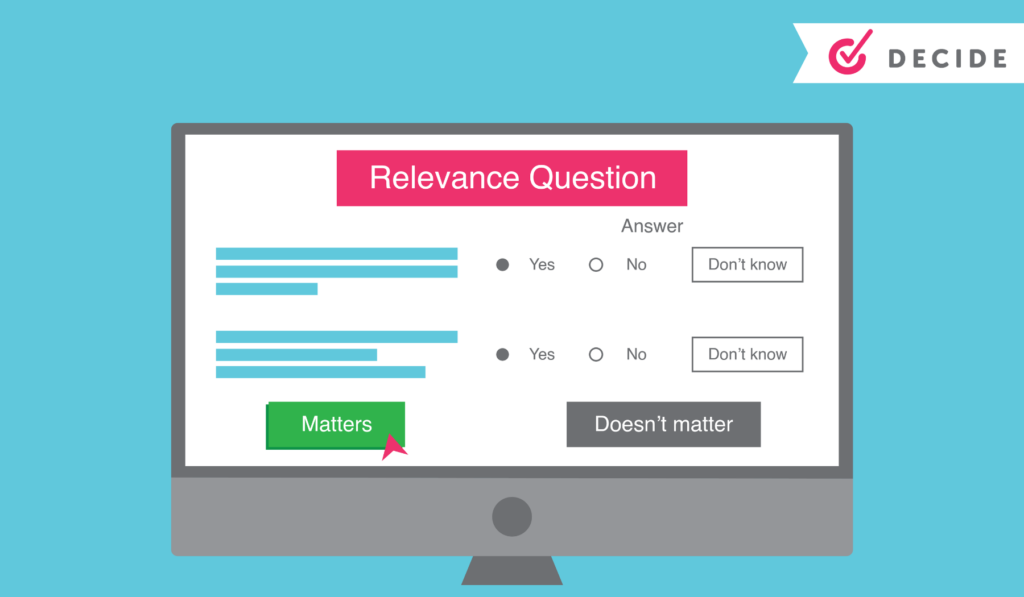
Regulatory analysis to help you decide
- For each requirement associated with a regulation, YouCompli creates a few relevance questions. Users may be asked, for instance, “Is your organization a Medicare provider?” These relevance questions are followed by tips generated by YouCompli to help make your decisions easier.
- We can do this because our analysts read entire regulations, flag relevant changes, and translate technical legal documents into easy-to-understand business requirements.
- If you decide the regulation is not relevant, YouCompli marks it “complete” and removes it from your active tasks.
- All our analysis is checked by Horty Springer, the nation’s leading health care law firm.
Get expertise from colleagues
Sometimes the relevance questions stretch beyond your expertise as a Compliance leader. In those cases, use YouCompli to get the answer from colleague with the right expertise.
- Use the workflow tool to assign a complex relevance question to a subject matter expert
- YouCompli allows you to maintain a directory of subject matter experts who provide compliance leadership within their departments
- The workflow tool also tracks responses and lets your colleague decline or answer the question right in the tool.
A complete audit trail for your relevance decisions
YouCompli tracks all of your relevance decisions over time, so you can see which regulations and changes applied to your organization and why (or why not!)
- All responses to decision criteria, including usernames and date stamps, are recorded in YouCompli to become part of the official record and the compliance audit trail
- The log also captures the reasons for rejecting the requirement or proceeding to the next phase of the workflow.
- YouCompli clients can access the complete audit trail at any time to review previous decisions and the reason for making that decision.
Great decisions help you manage regulatory changes
Once you know about a regulatory change and you’ve used YouCompli’s decision criteria to decide that a regulation applies to you, you’re ready to respond. YouCompli helps you manage the tasks necessary for compliance. And it helps you verify that your organization has put forth best efforts to stay in compliance.
Interested in how a healthcare system used YouCompli to decide which regulatory changes apply? Check out this case study from the Western Maryland Health System.
Collaboration Between Compliance and Risk: What is Permissible?
Compliance departments, generally speaking, guide staff and boards of directors to comply with the requirements, laws and regulations that govern the organization’s business. They also monitor for compliance via internal audits. Risk departments, on the other hand, address ways to mitigate risk to an organization through such activities as the evaluation and purchase of insurance policies. Given the broad nature of the scope of these two departments within the organization, when is compliance and risk collaboration permissible?
Possible collaborations
- Strategic planning: Collaboration here should include not only compliance and risk but the entire organization and the board of directors, if applicable.
- Disaster response and business continuity: As with strategic planning, disaster response and business continuity planning should also involve input and collaboration from all departments in the organization.
- General security and privacy : Here the compliance/privacy officer, information technology/security officer, and risk management director should all be included in the planning.
- Known security threat and/or breach incident: Compliance, information technology (IT), and risk management would all participate in mitigating a security threat or breach incident on the organization. Each would provide input and guidance on their respective areas of knowledge.
- Risk assessments, gap analysis and mitigation plans: Again, the development of these plans should include leaders from the entire organization; moreover, compliance and risk would specifically collaborate on the assessment, analysis and mitigation activities.
- General policy development: Compliance and risk staff can collaborate and provide feedback and input for all organization policies.
- Record and document retention schedule: Here compliance and risk can collaborate with legal counsel to ensure record and document retention policies comply with state and federal laws.
- Staff education: This is an area where compliance and risk can collaborate to provide training, whether it is done in person, virtually, by email or via online course.
Collaborations to vet and evaluate permissibility
- Security breach: As noted above, compliance, IT, and risk will work together once a security breach has been identified. It is important to ensure compliance addresses HIPAA related information and potential reporting requirements; IT evaluates the technical aspects of the breach; and risk focuses on reporting to the insurance carrier and mitigation strategies in conjunction with compliance and IT. These collaborative activities will usually take place under a breach coach or law firm to protect the confidential nature of the breach.
- Shared work areas: Depending on the confidential nature of discussions, say a lawsuit against the organization, it may or may not be appropriate for compliance staff to be privy to such information. So shared work areas should be closely evaluated.
- Shared staff: As with shared work areas, if a staff member such as a registered nurse (RN) is shared between the compliance and risk department, both leaders and the RN must remain in the scope of the job role in which they are working at the time.
- Reporting to the board: Typically, compliance reports to the organization’s leader (such as a CEO) but also has direct or dotted line reporting to the board of directors. Make sure any collaborations with other departments do not create potential conflicts of interest with reporting up this chain of command.
- Committee membership: As with the analysis discussed above, make sure to vet compliance staff member membership on the risk committee and vice versa to avoid any actual or potential conflicts of interest.
Goal
All organizations should work to develop a culture where permissible collaborations between compliance and risk occur. They should also make certain that staff feel comfortable calling the compliance or risk department with potential concerns while ensuring the staff not crossing any lines when it comes to compliance or risk department confidential matters or conflicts of interest.
PRACTICE TIP:
- Evaluate opportunities for the compliance department to collaborate with the risk management team, as noted above.
- Access youCompli to find resources which address required document and record retention requirements.
Denise Atwood, RN, JD, CPHRM
District Medical Group (DMG), Inc., Chief Risk Officer and Denise Atwood, PLLC
Disclaimer: The opinions expressed in this article or blog are the author’s and do not represent the opinions of DMG.

Denise Atwood, RN, JD, CPHRM has over 30 years of healthcare experience in compliance, risk management, quality, and clinical areas. She is also a published author and educator on risk, compliance, medical-legal and ethics issues. She is currently the Chief Risk Officer and Associate General Counsel at a nonprofit, multispecialty provider group in Phoenix, Arizona and Vice President of the company’s self-insurance captive.
Sign-up to never miss a compliance related article!
Manage your healthcare regulatory change process effectively and efficiently
YouCompli enables the compliance officers to assign ownership and oversight of tasks to different department heads, functional leaders, or specialists. The solution prompts users to accept, reject, or reassign the task by a stated deadline. Manage the rollout and accountability of new requirements with the best workflow in the business.
The Pandemic Is No Excuse: Enforcement Actions Taken by the Office for Civil Rights
We’ve known that enforcement actions were going to pick up again, even though many regulations are still waived or modified during the public health emergency. In the past few months, several decisions have been rendered by the Office for Civil Rights (OCR) which prove the point. Hospitals and other healthcare organizations need remain cautious and cognizant of exactly which regulations are being enforced, and make sure that existing procedures and policies are being followed.
Religious Rights
For example, OCR resolved a complaint against Prince George’s Hospital Center of the University of Maryland Medical System (UMMS). The complaint was raised by a woman who wanted to have a priest attend her critically injured husband during the pandemic. Despite the priest’s willingness to wear any necessary personal protective equipment (PPE), he was refused entry. UMMS implemented a new policy guaranteeing “adequate and lawful access to chaplains or clergy” in order to resolve the complaint.
A second religiously-based complaint was also resolved recently by OCR. In this complaint, filed by a civil rights group, a medical student at Staten Island University Hospital (SIUH) in New York City was ordered to shave his beard, which he kept for religious reasons. The hospital stated that this was in order to ensure his N95 respirator mask had a tight seal around his nose and mouth, even though he had passed a fit test. In resolving the complaint, SIUH provided the student with a Powered Air Purifying Respirator (PAPR) as a religious accommodation.
Privacy
OCR also recently resolved a HIPAA-based complaint. Lifespan Health System Affiliated Covered Entity (Lifespan ACE) in Rhode Island agreed to pay OCR $1,040,000 and to implement a corrective action plan to settle potential violations of the Health Insurance Portability and Accountability Act (HIPAA) Privacy and Security Rules related to the theft of an unencrypted laptop. Not only did the laptop contain electronic protected health information (ePHI) for 20,431 individuals, OCR found systemic noncompliance with HIPAA, including lack of encryption on laptops and a lack of device and media controls.
A Warning for Compliance
All these enforcement actions took place during the COVID-19 pandemic. The presence of the pandemic is not being taken as a reason for not proceeding with enforcement action. Compliance professionals need to be very aware of what regulations still apply, and how their organizations are continuing to stay within the scope of existing regulations.
See YouCompli in Action
Easier, faster, more effective compliance is possible
The New Office of Burden Reduction and Health Informatics: Implications for Healthcare Compliance
You may have heard that, last week, the Centers for Medicare & Medicaid Services (CMS) announced the creation of a new office: the “Office of Burden Reduction and Health Informatics.”
What exactly is this new office supposed to do? According to the press release from CMS, the intent is “to unify the agency’s efforts to reduce regulatory and administrative burden and to further the goal of putting patients first.”
All well and good. But what does that actually mean?
Value-Based Care
Here’s one thing that CMS says clearly. They are “committed to leveraging the significant flexibilities introduced in response to the COVID-19 pandemic as we continue to lead the rapid transformation to value-based healthcare.”
We’ve all been hearing about value-based care for years. (Here’s a piece from 2016, for example.) The pace of change hasn’t been particularly speedy, and the pandemic has disrupted most big transformative plans, especially in healthcare.
That said, the Department of Health and Human Services (HHS) is still committed to value-based care. If reducing or streamlining the regulatory environment is necessary in order to make this change happen, you can bet that HHS and CMS will do it.
What specific regulations will CMS change in order to make this happen? That remains to be seen. Recently, CMS did announce that they will be maintaining at least some of the regulatory changes related to telehealth.
Which ones? We know of one rule change that CMS has announced: the proposed physician fee schedule rule, which should come out in July, will include proposals to permanently expand coverage for telehealth services. As of this writing, the rule has not been published, and CMS has not announced details.
With that exception, however, there hasn’t been a lot of movement on specific regulations that could be helpful. In fact, our observations suggest that most regulators are moving back to business as usual. If CMS has plans to streamline regulations to enable the transformation to value-based care, they are keeping those plans very close to the vest.
Improved Review
However, CMS commits clearly to increasing the number of stakeholders – including clinicians, providers and health plans – that it engages with when assessing the impact of new regulations.
This could be a welcome change for compliance professionals, as a more comprehensive assessment of regulatory impact could result in a regulatory environment that’s a lot easier to work within. Clearer regs with reduced expectations would mean less work required by the clinical and revenue cycle staff in your organization.
And that would mean less time spent following up and trying to get staff to do the work.
Health Informatics
CMS has also committed – as indicated in the second half of the new office’s name – to further implement health informatics. The idea here is to effectively use health data in order to provide better care.
CMS gives this as a specific example: “to create new tools that allow patients to own and carry their personal health data with them seamlessly, privately, and securely throughout the health care system.”
This proposal has obvious advantages for both patients and providers. But it could cause significant headaches for compliance.
Staying in compliance with an EHR system for just one health system is challenging enough. What CMS is proposing is an EHR system that applies across all Medicare and Medicaid beneficiaries. This would be much more complicated! The HIPAA implications alone could be staggering.
So, the use of health informatics could make the work of compliance much more challenging. We can all expect that there will be more data available and being used, and more complex tools to manage it. This trend exists across almost all industries, and healthcare is not going to be an exception.
In a highly regulated environment like healthcare, however, big data and big data tools will need to be monitored very carefully. There are a lot of ways that data tools could violate regulatory requirements. If compliance professionals aren’t careful, software and other tools could be put in place that expose the organization to high levels of risk.
Staying Up to Date
As of this writing, there is limited information as to what the Office of Burden Reduction and Health Informatics will be doing for the US healthcare system. It has a broad mandate, with unclear specifics.
There is a possibility that the office will make compliance easier, by more effectively assessing the impact of regulations before imposing them. There is also a (stronger) possibility that it may make compliance more challenging, by creating wide-ranging technological systems that compliance officers will need to monitor carefully.
As new regulations are issued, and new announcements are made, we’ll be keeping you updated. youCompli customers always have access to the latest regulatory changes as they come out and will be well-positioned to adapt to the environment created by his new office.
See YouCompli in Action
Easier, faster, more effective compliance is possible
Not All COVID-19 Regulations Are Created Equal
You’re struggling to keep up with all the regulatory changes that COVID-19 has created.
Many of these changes have been short and straightforward… but not all of them.
After analyzing one CMS reg (85 FR 27550), we created a 19-page policy document!
The reg’s primary purpose expanded the range of practitioners who can order — and thus be compensated by Medicare and Medicaid — home health services. It also covers a wide range of other revisions for testing, telehealth, medical equipment, and so on.
Our system broke the regulation down into its core requirements — that is, the pieces of the reg that healthcare compliance and clinical professionals need to know about. Then it was reassembled into this document and placed in an order that makes sense.
You can view the whole document by clicking this link.
Every change to a previous procedure is highlighted in red, and it includes hyperlinks to skip around.
Everything is written in clear language, so it’s easy to follow and implement.
Want us to do the same for your organization and the regulations you’re managing? Set up a quick meeting here and let’s get started.
See YouCompli in Action
Easier, faster, more effective compliance is possible
Earning the Gold Seal of Approval from the Joint Commission
Revised September 2022
Complying with the latest regulations will always be a critical priority for healthcare compliance professionals. But earning approval from The Joint Commission, the recognized global leader for health care accreditation, is growing in importance across healthcare organizations, including hospitals, physician group practices, surgery centers, and other treatment facilities.
This accreditation, known as The Gold Seal of Approval®, acknowledges an organization’s dedication to providing quality care and services to patients. Some states require health care organizations to be accredited by the Commission in order to participate in particular insurance programs.
If a healthcare organization is accredited by The Joint Commission, it may be deemed to exceed Centers for Medicare and Medicaid (CMS) requirements, along with state law requirements. Additionally, with the public’s attention increasingly focused on becoming informed consumers, earning accreditation also offers organizations a competitive edge.
Meet the Joint Commission
The Joint Commission is an independent, not-for-profit organization based in Illinois. Founded more than 65 years ago, the Commission provides an unbiased assessment of a health care organization’s quality achievements in patient care and safety.
It offers the following accreditation programs:
- Ambulatory Care Accreditation
- Behavioral Health Care Accreditation
- Critical Access Hospital Accreditation
- Home Care Accreditation
- Hospital Accreditation
- Laboratory Services Accreditation
- Nursing Care Center Accreditation
- Office-Based Surgery Accreditation
In addition, The Joint Commission offers 20 different certifications for a variety of clinical programs and services.
Understand the Accreditation Process
The Commission’s standards set expectations for an organization’s performance that are reasonable, achievable, and measurable. Its on-site surveys are rigorous and are customized for each organization and its efforts to improve patient outcomes. And the start of a survey is usually unannounced.
During an on-site survey, Commission surveyors perform their evaluation by:
- Tracing the care delivered to patients, residents, or individuals served
- Reviewing the information and documentation provided by the organization
- Observing and interviewing staff and, when appropriate, patients
The Commission provides a Summary of Survey Findings Report at the conclusion of the on-site survey, with a final accreditation decision made at a later date. Surveyors could recommend:
- Preliminary accreditation
- Accreditation
- Accreditation with follow-up survey
- Preliminary denial of accreditation
- Denial of accreditation
An organization’s accreditation is continuous as long as it has a full, unannounced survey within 36 months of the previous survey and it meets all accreditation-related requirements.
Benefits from Accreditation
The Gold Seal of Approval is a way to let medical professionals, government regulators, and patients know that an organization stands for quality care, and that it’s always seeking ways to identify known or unknown risks to patient safety.
For example, healthcare organizations that want to participate in Medicare have to be certified to have met specific CMS quality-related standards. If the organization is accredited by The Joint Commission, CMS will have deemed the entity to have met or exceeded these requirements. That means the organization is not subject to Medicare’s survey and certification process because it has already gone through the Commission’s survey process.
Additionally, being Commission-accredited may allow the organization to be exempt from meeting state law survey or quality or requirements. Here you want to be sure and check your state laws to see if they exempt entities accredited by The Joint Commission.
In what other ways can an organization benefit from Joint Commission accreditation?
- It can earn various Joint Commission certifications for continued improvement and maintaining performance excellence
- It can connect with other like-minded organizations to collaborate on issues affecting the quality and safety of patient care
- It can attract more qualified personnel who prefer to serve in a prestigious environment
Earning Accreditation Means Maintaining Compliance
Earning the Joint Commission’s Gold Seal of Approval depends on a strong culture of compliance. Organizations that are challenged to manage compliance, or effectively demonstrate compliance, are unlikely to meet the Joint Commission’s rigorous standards. (Read more about Compliance Culture on the YouCompli blog.)
A culture of compliance is a commitment throughout all levels of an organization to do the right thing and do things right. When an organization has a strong culture of compliance, there is a spillover effect to obtaining and maintaining Commission accreditation. Employees see their leaders ensuring the organization is maintaining compliance with elevated standards. Additionally, they see their leaders making business decisions based on organizational policy requirements. The end result is actions being taken that demonstrate leading by example and modeling that behavior to employees.
The Gold Seal of Approval accreditation is an important acknowledgment of an organization’s dedication to providing quality care and services to patients. The effort to earn this accreditation is certainly significant, but the payoff in terms of reputation, recruiting and deeming status is worth the effort. Not only that, the process of earning accreditation can help you uncover opportunities to further shape your culture of compliance so that a mindset of always doing the right thing permeates all levels of your organization. All of that is good for the long-term health of your business – and your patients.
The accreditation process requires significant metrics to demonstrate the effectiveness of your compliance program, YouCompli can help you verify that you took the proper steps to comply with the regulations that apply to you. Find out how.

Jerry Shafran is the founder and CEO of YouCompli. He is a serial entrepreneur who builds on a solid foundation of information technology and network solutions. Jerry launches, manages, and sells software and content solutions that simplify complex work. His innovations enable professionals to focus on their core business priorities.
Never Miss a Compliance Related Article
Highlights from OIG’s Semi-Annual Report to Congress
Late last week, the HHS OIG made available its semi-annual report to Congress summarizing OIG activities occurring from October 1, 2017 to March 31, 2018. As one might expect, OIG continues to commit resources to enforcement-related activities and to improve its data analytics capabilities. A few of the “headlines” from an enforcement perspective include: Criminal […]
Continue reading