Improve patient care and protect your healthcare organization under evolving telehealth compliance requirements today. How to prepare for regulatory change.
Continue readingTrust in healthcare compliance programs
Four ways to build a healthy culture of compliance. Help your clinical and operational colleagues see compliance as foundational to your healthcare organization
Continue readingCompliance officer effectiveness takes a special blend of skills
Highly effective board committees know their oversight responsibilities. After a four-year investigation, Caremark pled guilty to felony mail fraud and entered into numerous settlement agreements. The primary allegation was that the board failed to make reasonable inquiries and take appropriate action to prevent certain systemic compliance failures.
Continue readingFour Power Skills for Influence
Compliance helps healthcare organizations mitigate risk by building strong relationships and leading through influence for effective regulatory change management
Continue readingNursing-shortage solutions come with licensure challenges
The nursing shortage in the US was bad before the pandemic started. Now after the double whammy of a two-year pandemic and an aging population, it’s even worse.
The American Nursing Association estimates that this year will see more than 100,000 unfilled nursing jobs, “more than any other profession.”
Hospitals have traditionally brought in “nurse travelers” from outside their service areas and their states to comply with state staffing requirements. In 2000, the Nursing Licensure Compact permitted nurses licensed in one participating state to practice in other participating states. In 2018 the Enhanced Nursing Licensure Compact (eNLC) added some requirements, such as state and federal fingerprint-based criminal background checks.
With Vermont having started implementation February 1, 36½ states and territories are eNLC participants. Ohio has joined but won’t implement participation until January 2023. Pennsylvania and the US Virgin Islands have joined but have not yet set implementation dates. The half is Guam, which recognizes eNLC licenses but whose nurses won’t be able to apply for one until later this year.
Interstate licensing considerations for traveling nurses
Nurse burnouts, quits, and anticipated retirements (500,000 RNs this year) have only added to the need for hiring travelers to fill the gaps. But before you do, there are potential pitfalls to watch out for:
- Does your state belong to the eNLC? Does the nurse’s home state? If not, what are the licensure requirements for nurses with out-of-state licenses?
- If your state has passed eNLC legislation, have they implemented it yet? If not, have they set a date for doing so?
- If eNLC legislation is pending in your state, what’s its status?
- Do you have a process in place for checking and verifying out-of-state licenses?
- If your state is not an eNLC participant, what are its regulations regarding out-of-state licensure?
- What if nurses you hired as travelers join your contracted staff and move to your state? Have you a process for making sure they updated their licenses from multi-state to your state? Are the in-state licenses current? If not, you’ll have been providing patient care services without a license.
The expanding availability of out-of-state nurses can be hugely helpful for solving short-term nursing shortages. An audit of your practices against current regulations and compacts is a great first step in determining where and how to use traveling nurses in a compliant way.
Do you have a system in place to manage regulatory changes? Having a solution that researches and analyzes regulatory changes, translates them into model procedures, and has a top healthcare law firm validate them can really pay. Read more about YouCompli’s regulatory monitoring process or schedule a demo.
Get the latest article in your email
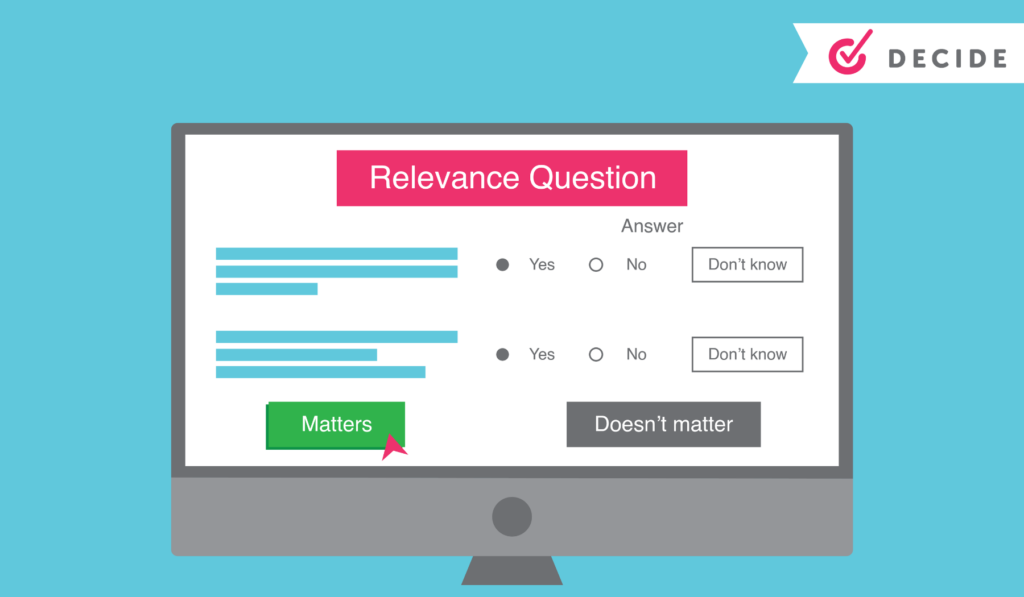
Decide: YouCompli helps your organization make easy regulatory decisions
Before YouCompli, Compliance Officer Scott Borsuk said he “probably spent six to eight hours a week reading regulations, then copying and pasting them” to share with colleagues. Read the Western Maryland Health System case study.
“It’s not enjoyable reading,” Borsuk noted.
But he had to read closely to be sure he properly analyzed the regulation to see if it applied to him.
Simplify decision-making
“We were not confident that we were catching everything, we had the documents but didn’t know if we missed anything. At the end of the day, we didn’t know if we were making the right changes or not.” – Scott Borsuk, Chief Compliance Officer
Borsuk knew he needed a better system and a stronger approach to managing regulatory change. That’s where YouCompli came in. With YouCompli, Borsuk can easily decide if a regulation applies to his hospital system and how to comply.
YouCompli makes it easy for you to decide which regulatory changes apply to your organization and which tasks need to be performed in order to comply.
In this clip Scott Borsuk explains what regulatory change management is, and how YouCompli assisted his hospital system in achieving desired results.
Watch more videos on this topic here and see how YouCompli can help your organization
Regulatory analysis to help you decide
- For each requirement associated with a regulation, YouCompli creates a few relevance questions. Users may be asked, for instance, “Is your organization a Medicare provider?” These relevance questions are followed by tips generated by YouCompli to help make your decisions easier.
- We can do this because our analysts read entire regulations, flag relevant changes, and translate technical legal documents into easy-to-understand business requirements.
- If you decide the regulation is not relevant, YouCompli marks it “complete” and removes it from your active tasks.
- All our analysis is checked by Horty Springer, the nation’s leading health care law firm.
Get expertise from colleagues
Sometimes the relevance questions stretch beyond your expertise as a Compliance leader. In those cases, use YouCompli to get the answer from colleague with the right expertise.
- Use the workflow tool to assign a complex relevance question to a subject matter expert
- YouCompli allows you to maintain a directory of subject matter experts who provide compliance leadership within their departments
- The workflow tool also tracks responses and lets your colleague decline or answer the question right in the tool.
A complete audit trail for your relevance decisions
YouCompli tracks all of your relevance decisions over time, so you can see which regulations and changes applied to your organization and why (or why not!)
- All responses to decision criteria, including usernames and date stamps, are recorded in YouCompli to become part of the official record and the compliance audit trail
- The log also captures the reasons for rejecting the requirement or proceeding to the next phase of the workflow.
- YouCompli clients can access the complete audit trail at any time to review previous decisions and the reason for making that decision.
Great decisions help you manage regulatory changes
Once you know about a regulatory change and you’ve used YouCompli’s decision criteria to decide that a regulation applies to you, you’re ready to respond. YouCompli helps you manage the tasks necessary for compliance. And it helps you verify that your organization has put forth best efforts to stay in compliance.
Interested in how a healthcare system used YouCompli to decide which regulatory changes apply? Check out this case study from the Western Maryland Health System.
Helping hospital systems know how to implement the No Surprises Act
Hospital systems knows regulatory changes created by the No Surprises Act and what to do for a successful implementation.
Continue readingHospital system elevates its approach to deciding when regulations are relevant
An endless stream of new and changing laws requires chief compliance officer, Scott Borsuk to decide relevant healthcare regulations for the hospital
Continue readingCompliance function serves as trusted business partner and helps colleagues verify their coding and procedures are up-to-date
Compliance function serves as trusted business partner and helps colleagues verify their coding and procedures are up-to-date
Continue reading