Four ways to build a healthy culture of compliance. Help your clinical and operational colleagues see compliance as foundational to your healthcare organization
Continue readingFour Power Skills for Influence
Compliance helps healthcare organizations mitigate risk by building strong relationships and leading through influence for effective regulatory change management
Continue readingEstablishing a regulatory change management process for healthcare
Stakeholder relationships and standard regulatory change management processes are critical for effective healthcare compliance
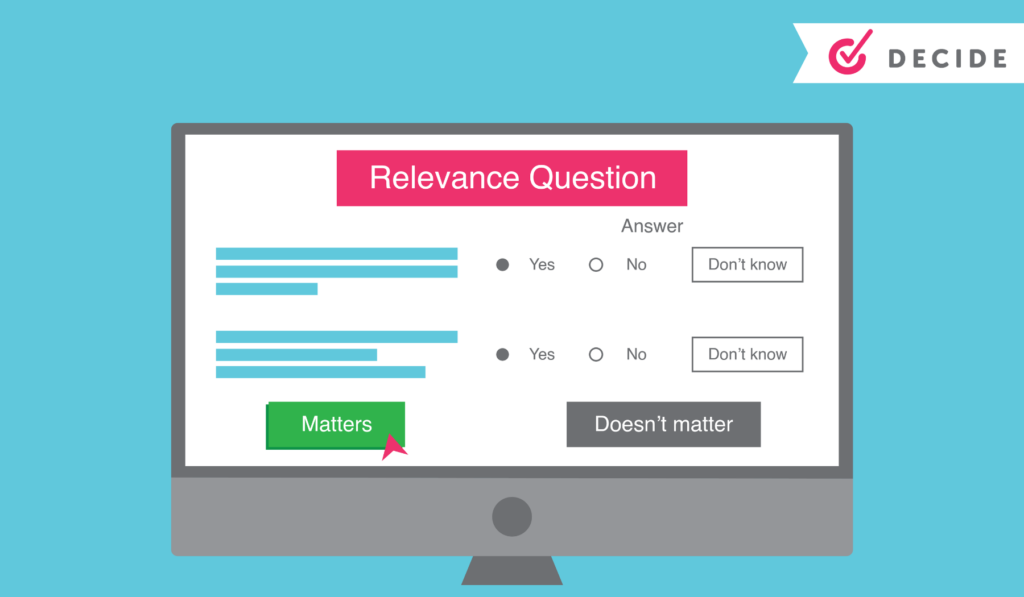
Continue readingDecide: YouCompli helps your organization make easy regulatory decisions
Before YouCompli, Compliance Officer Scott Borsuk said he “probably spent six to eight hours a week reading regulations, then copying and pasting them” to share with colleagues. Read the Western Maryland Health System case study.
“It’s not enjoyable reading,” Borsuk noted.
But he had to read closely to be sure he properly analyzed the regulation to see if it applied to him.
Simplify decision-making
“We were not confident that we were catching everything, we had the documents but didn’t know if we missed anything. At the end of the day, we didn’t know if we were making the right changes or not.” – Scott Borsuk, Chief Compliance Officer
Borsuk knew he needed a better system and a stronger approach to managing regulatory change. That’s where YouCompli came in. With YouCompli, Borsuk can easily decide if a regulation applies to his hospital system and how to comply.
YouCompli makes it easy for you to decide which regulatory changes apply to your organization and which tasks need to be performed in order to comply.
In this clip Scott Borsuk explains what regulatory change management is, and how YouCompli assisted his hospital system in achieving desired results.
Watch more videos on this topic here and see how YouCompli can help your organization
Regulatory analysis to help you decide
- For each requirement associated with a regulation, YouCompli creates a few relevance questions. Users may be asked, for instance, “Is your organization a Medicare provider?” These relevance questions are followed by tips generated by YouCompli to help make your decisions easier.
- We can do this because our analysts read entire regulations, flag relevant changes, and translate technical legal documents into easy-to-understand business requirements.
- If you decide the regulation is not relevant, YouCompli marks it “complete” and removes it from your active tasks.
- All our analysis is checked by Horty Springer, the nation’s leading health care law firm.
Get expertise from colleagues
Sometimes the relevance questions stretch beyond your expertise as a Compliance leader. In those cases, use YouCompli to get the answer from colleague with the right expertise.
- Use the workflow tool to assign a complex relevance question to a subject matter expert
- YouCompli allows you to maintain a directory of subject matter experts who provide compliance leadership within their departments
- The workflow tool also tracks responses and lets your colleague decline or answer the question right in the tool.
A complete audit trail for your relevance decisions
YouCompli tracks all of your relevance decisions over time, so you can see which regulations and changes applied to your organization and why (or why not!)
- All responses to decision criteria, including usernames and date stamps, are recorded in YouCompli to become part of the official record and the compliance audit trail
- The log also captures the reasons for rejecting the requirement or proceeding to the next phase of the workflow.
- YouCompli clients can access the complete audit trail at any time to review previous decisions and the reason for making that decision.
Great decisions help you manage regulatory changes
Once you know about a regulatory change and you’ve used YouCompli’s decision criteria to decide that a regulation applies to you, you’re ready to respond. YouCompli helps you manage the tasks necessary for compliance. And it helps you verify that your organization has put forth best efforts to stay in compliance.
Interested in how a healthcare system used YouCompli to decide which regulatory changes apply? Check out this case study from the Western Maryland Health System.
12 key metrics for compliance officers looking to move their culture forward
Culturally impactful metrics emphasize getting healthcare compliance officers in the right rooms – ahead of regulatory change or organizational growth.
Continue readingHelping hospital systems know how to implement the No Surprises Act
Hospital systems knows regulatory changes created by the No Surprises Act and what to do for a successful implementation.
Continue readingPrivacy protection: When our colleagues are our patients
How can you protect personal health information (PHI), medical records, and patient communication when the provider is also the patient?
Continue readingStark Law and its revisions benefit patients
Recent changes to Stark aim to increase coordination of patient care, modernize, and clarify rules related to the law.
Continue readingFive tips to help providers comply with Stark
The Stark Law creates a whole set of antikickback rules that providers must understand and actively work to comply with. And with all its good intentions, the Stark Law is incredibly restrictive. In fact, even the U.S. Court of Appeals for the 4th Circuit noted that “even for the well-intentioned healthcare provider, the Stark law has become a booby trap rigged with strict liability and potentially ruinous exposure.”
The Centers for Medicare and Medicaid (CMS) and Congress have taken steps to clear up confusion and loosen the rules in some cases (See our article on exceptions for value-based care). Still, your Compliance team has a tremendous responsibility to make sure that policies match the rules and that providers understand and follow the policies.
Policies match the Stark rules
Changes to the Stark Law have been coming out practically since the law was enacted. The law, which aims to protect against kickbacks and self-referrals, has gotten complicated in the details. Congress issues amendments to help the law catch up to changing business practices. Healthcare organizations may have written policies that facilitated compliance originally. However, those may be completely out-of-date if they weren’t keeping up with the changes in the law.
For example, CMS has introduced modifications that addressed challenges with value-based care and resolve issues restricting coordinated care and health data exchange. Another modification to the law was allowing healthcare providers to accept cybersecurity tech donations from stakeholders.
While the compliance officer enforces the policies, he or she doesn’t have to live them the way those in operations do. Getting input from key stakeholders such as providers, Risk Management, and others in the C-suite can help ensure that final policies are clear. This early feedback and engagement can also help identify how the policy or regulatory changes will affect the individuals who must operate under them. Lastly, they can help identify potential operational conflicts with new policies or regulatory changes.
(See how YouCompli delivers model policies and procedures that help your organization comply.)
Providers following the Stark policies
With compliant policies in place, it’s time to help providers understand how to follow them. This is where communicating what certain key terms in a policy or regulation means in the context of the provider’s particular work becomes critically important.
Compliance officers know that “the road to success is going to run through quality of care,” says Harry Nelson, health care attorney at Nelson Hardiman. “Compliance isn’t the internal police that slows things down, but a strategic part of growth.” When it comes to making sure providers understand how to follow policies, the compliance officer has to look at the language of the policy from the providers’ perspective, not that of the compliance officer.
Here are five steps to help providers understand and follow Stark-compliant policies:
- Engage your operational leaders. Make sure the president and CEO understand the nature and intent behind Stark limitations so they can help explain and reinforce them. Give situational examples they can relate to so they understand what the key terminology means.
- Invest in training and communication. One email won’t do it with changes to Stark-related policies. Engage providers in small groups, in writing, and in person to explain nuances and answer questions about tricky scenarios. Whenever possible, use real-world scenarios to help illustrate how the regulations and policies impact them. Education and training should also be routine and ongoing with key stakeholders.
- Get feedback. Regularly check in to gather feedback from your leaders. Find out if the implemented tools and procedures are working for them, as well as to identify challenges they face. This step will help you see areas where the words on paper mean something the compliance officer had not thought of. Adapt procedures and tools if necessary.
- Encourage people to ask questions. Make sure providers and your operational leaders alike know they can use you as a sounding board for grey areas or possible violations. It’s much better if they proactively ask if a proposed arrangement is compliant. Otherwise, they may have to unwind a relationship if they find out it is not compliant.
- Promote awareness to prevent future mistakes. Once an error is made, chances are it will reoccur and lead to additional violations. As you are addressing errors, promote awareness to prevent future mistakes. For example, when you are communicating the fact that a mistake was made, go the extra step to what caused it. This will be an opportunity to find out where their confusion was and use that insight to update policies or training.
Stark compliance starts with knowing about changes to the regulations and continues with crafting policies that providers can understand and follow. Involving stakeholders in policy creation and training, and engaging tech systems to reinforce the lessons will support the long-term success of Stark-compliant policies.
Do you have the tools you need to recognize and manage regulatory change across your organization? Find out how YouCompli can help you manage and coordinate your response to regulatory change or schedule a demo.
Subscribe for blog updates